List of Adverse Events in Pfizer's Covid-19 mRNA Vaccine Post Marketing Experience Report
Download Pfizer's report which lists adverse events from their own post analysis of the BNT162B2 Covid-19 mRNA ‘vaccine’.

Below is Pfizer's report which was to be hidden for 75 years. The Appendix lists adverse events from their analysis of the BNT162B2 Covid-19 mRNA ‘vaccine’. (pp 30-38)
Former Blackrock Fund Manager Edward Dowd tracked disability and death data from 4th quarter 2022 UK & US life group life insurers' reported a surge in claims from the young, working age demographic since the ‘vaccine’ and ‘booster’ rollouts. Deaths and disabilities have continued to increase in 2024.
List of Adverse Events Reported by Pfizer
• 1p36 deletion syndrome.
1p36 deletion syndrome is a congenial genetic disorder that affects fetuses and deletes part of their chromosomes, causing severe intellectual disabilities. Most affected individuals do not speak, or speak only a few words. They may have temper tantrums, bite themselves, or exhibit other behaviourial problems.
• 2-Hydroxyglutaric aciduria.
• 5'nucleotidase increased.
A
• Acoustic neuritis.
• Acquired C1 inhibitor deficiency.
• Acquired epidermolysis bullosa.
• Acquired epileptic aphasia.
• Acute cutaneous lupus erythematosus.
• Acute disseminated encephalomyelitis.
• Acute encephalitis with refractory, repetitive partial seizures.
• Acute febrile neutrophilic dermatosis.
I had this I think it’s the same - Acute febrile neutrophillic disease or sweet syndrome - you need a course of steroids and olive leaf extract
— martin pitchford (@PitchfordMartin) August 27, 2022
• Acute flaccid myelitis.
• Acute haemorrhagic leukoencephalitis.
• Acute haemorrhagic oedema of infancy.
• Acute kidney injury.
• Acute macular outer retinopathy.
• Acute motor axonal neuropathy.
• Acute motor-sensory axonal neuropathy.
• Acute myocardial infarction.
Myocarditis and acute myocardial infarction (AMI) have been reported after COVID-19 messenger ribonucleic acid vaccination.
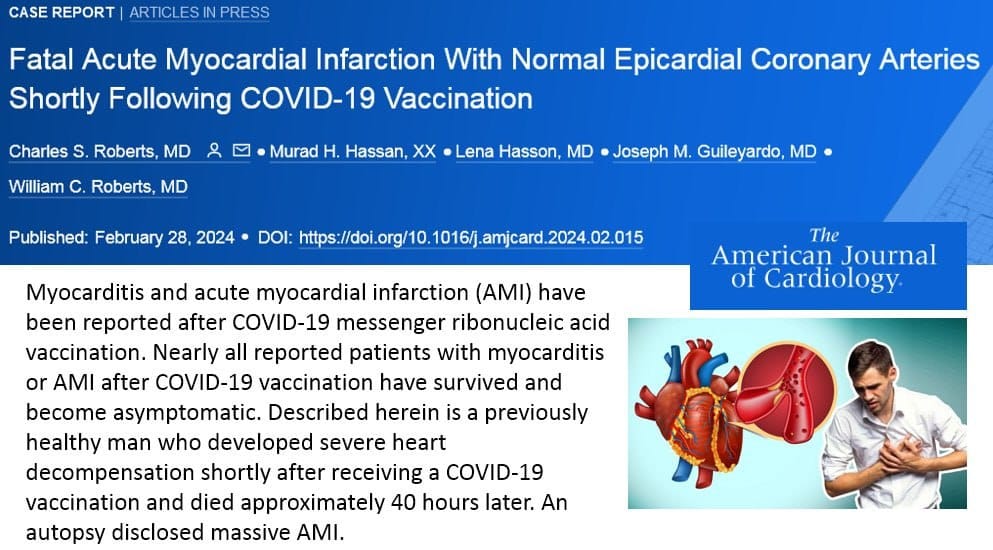
Described herein is a previously healthy man who developed severe heart decompensation shortly after receiving a COVID-19 vaccination and died approximately 40 hours later. An autopsy disclosed massive AMI.
Case report of 7 year old child due to pericarditis and myocarditis after the mRNA vaccine against COVID-19.
• Acute respiratory distress syndrome.
Acute respiratory distress syndrome (ARDS) is a serious lung condition that causes low blood oxygen. People who develop ARDS are usually ill due to another disease or a major injury. In ARDS, fluid builds up inside the tiny air sacs of the lungs, and surfactant breaks down.
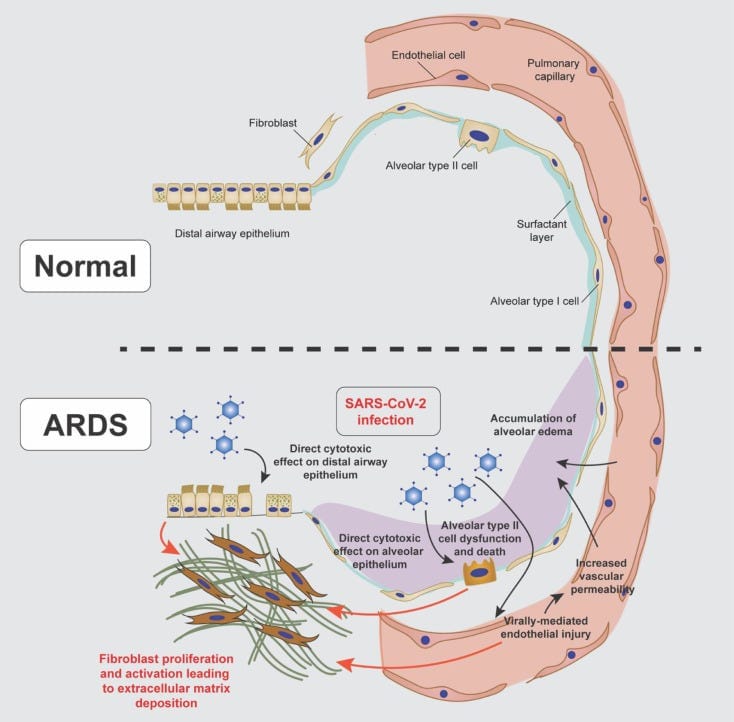
Mechanisms of fibroproliferation in COVID-19-induced ARDS: SARS-CoV-2 infection can lead to acute respiratory distress syndrome (ARDS) during which severe fibroproliferation can occur.
SARS-CoV-2 and its Spike Protein induce aberrant repair mechanisms in multiple organs. The result of these aberrant actions is fibrosis and ossification in organs.
• Acute respiratory failure.
• Addison's disease.
• Administration site thrombosis
• Administration site vasculitis.
• Adrenal thrombosis.
• Adverse event following immunisation.
• Ageusia.
• Agranulocytosis.
• Air embolism.
• Alanine aminotransferase abnormal.
• Alanine aminotransferase increased.
• Alcoholic seizure.
• Allergic bronchopulmonary mycosis.
• Allergic oedema.
• Alloimmune hepatitis.
• Alopecia areata.
• Alpers disease.
• Alveolar proteinosis.
• Ammonia abnormal.
• Ammonia increased.
• Amniotic cavity infection.
• Amygdalohippocampectomy.
• Amyloid arthropathy.
• Amyloidosis.
Amyloidoses are a group of debilitating and often fatal diseases in which fibrillar protein aggregates are deposited in the extracellular spaces of a range of tissues. (See paper here)
Spike Protein Endothelial Phase (SPED ) is the first step in a disease process which is, ultimately, a disease of the Extracellular Matrix. The Spike Protein invades the extracellular matrix via the Endothelium and then precipitates amyloids systemically, through all major organs and systems.
• Amyloidosis senile.
• Anaphylactic reaction.
• Anaphylactic shock.
• Anaphylactic transfusion reaction.
• Anaphylactoid reaction.
• Anaphylactoid shock.
• Anaphylactoid syndrome of pregnancy.
• Angioedema;Angiopathic neuropathy.
• Ankylosing spondylitis.
• Anosmia;Antiacetylcholine receptor antibody positive.
• Anti-actin antibody positive.
• Anti-aquaporin-4 antibody positive.
• Anti-basal ganglia antibody positive.
• Anti-cyclic citrullinated peptide antibody positive.
• Anti-epithelial antibody positive.
• Anti-erythrocyte antibody positive.
• Anti-exosome complex antibody positive.
• Anti- GAD antibody negative.
• Anti-GAD antibody positive.
• Anti-ganglioside antibody positive.
• Antigliadin antibody positive.
• Anti-glomerular basement membrane antibody positive.
• Anti-glomerular basement membrane disease.
• Anti-glycyl-tRNA synthetase antibody positive.
• Anti-HLA antibody test positive.
• Anti-IA2 antibody positive.
• Anti-insulin antibody increased.
• Anti-insulin antibody positive.
• Anti-insulin receptor antibody increased.
• Anti- insulin receptor antibody positive.
• Anti-interferon antibody negative.
• Anti-interferon antibody positive.
• Anti-islet cell antibody positive.
• Antimitochondrial antibody positive.
• Anti-muscle specific kinase antibody positive.
• Anti-myelin-associated glycoprotein antibodies positive.
• Anti-myelin-associated glycoprotein associated polyneuropathy.
• Antimyocardial antibody positive;Anti-neuronal antibody positive.
• Antineutrophil cytoplasmic antibody increased.
• Antineutrophil cytoplasmic antibody positive.
• Anti-neutrophil cytoplasmic antibody positive vasculitis.
• Anti-NMDA antibody positive.
• Antinuclear antibody increased.
• Antinuclear antibody positive.
• Antiphospholipid antibodies positive.
• Antiphospholipid syndrome.
• Anti-platelet antibody positive.
• Anti-prothrombin antibody positive.
• Antiribosomal P antibody positive.
• Anti-RNA polymerase III antibody positive.
• Anti-saccharomyces cerevisiae antibody test positive.
• Anti-sperm antibody positive;Anti-SRP antibody positive.
• Antisynthetase syndrome.
• Anti-thyroid antibody positive.
• Anti-transglutaminase antibody increased.
• Anti-VGCC antibody positive.
• Anti- VGKC antibody positive.
• Anti-vimentin antibody positive.
• Antiviral prophylaxis.
• Antiviral treatment.
• Anti-zinc transporter 8 antibody positive.
• Aortic embolus.
• Aortic thrombosis.
• Aortitis.
• Aplasia pure red cell.
• Aplastic anaemia.
• Application site thrombosis.
• Application site vasculitis.
• Arrhythmia.
• Arterial bypass occlusion.
• Arterial bypass thrombosis.
• Arterial thrombosis.
• Arteriovenous fistula thrombosis.
• Arteriovenous graft site stenosis.
• Arteriovenous graft thrombosis.
• Arteritis.
• Arteritis coronary.
• Arthralgia.
• Arthritis.
• Arthritis enteropathic.
• Ascites.
• Aseptic cavernous sinus thrombosis.
• Aspartate aminotransferase abnormal.
• Aspartate aminotransferase increased.
• Aspartate-glutamate-transporter deficiency.
• AST to platelet ratio index increased.
• AST/ALT ratio abnormal.
• Asthma.
• Asymptomatic COVID- 19.
• Ataxia.
• Atheroembolism.
• Atonic seizures.
• Atrial thrombosis.
• Atrophic thyroiditis.
• Atypical benign partial epilepsy.
• Atypical pneumonia.
• Aura;Autoantibody positive.
• Autoimmune anaemia.
• Autoimmune aplastic anaemia.
• Autoimmune arthritis.
• Autoimmune blistering disease.
• Autoimmune cholangitis.
• Autoimmune colitis.
• Autoimmune demyelinating disease.
• Autoimmune dermatitis.
• Autoimmune disorder.
• Autoimmune encephalopathy.
• Autoimmune endocrine disorder.
• Autoimmune enteropathy.
• Autoimmune eye disorder.
• Autoimmune haemolytic anaemia.
• Autoimmune heparin-induced thrombocytopenia.
• Autoimmune hepatitis.
• Autoimmune hyperlipidaemia.
• Autoimmune hypothyroidism.
• Autoimmune inner ear disease.
• Autoimmune lung disease.
• Autoimmune lymphoproliferative syndrome.
• Autoimmune myocarditis;Autoimmune myositis.
• Autoimmune nephritis.
• Autoimmune neuropathy.
• Autoimmune neutropenia.
• Autoimmune pancreatitis.
• Autoimmune pancytopenia.
• Autoimmune pericarditis.
• Autoimmune retinopathy.
• Autoimmune thyroid disorder.
• Autoimmune thyroiditis.
• Autoimmune uveitis.
• Autoinflammation with infantile enterocolitis.
• Autoinflammatory disease.
• Automatism epileptic.
• Autonomic nervous system imbalance.
• Autonomic seizure.
• Axial spondyloarthritis.
• Axillary vein thrombosis.
• Axonal and demyelinating polyneuropathy.
• Axonal neuropathy.
B
• Bacterascites.
• Baltic myoclonic epilepsy.
• Band sensation.
• Basedow's disease.
• Basilar artery thrombosis.
• Basophilopenia.
• B-cell aplasia.
• Behcet's syndrome.
• Benign ethnic neutropenia.
• Benign familial neonatal convulsions.
• Benign familial pemphigus.
• Benign rolandic epilepsy.
• Beta-2 glycoprotein antibody positive.
• Bickerstaff's encephalitis
• Bile output abnormal.
• Bile output decreased.
• Biliary ascites.
• Bilirubin conjugated abnormal.
• Bilirubin conjugated increased.
• Bilirubin urine present.
• Biopsy liver abnormal.
• Biotinidase deficiency.
• Birdshot chorioretinopathy.
• Blood alkaline phosphatase abnormal.
• Blood alkaline phosphatase increased.
• Blood bilirubin abnormal.
• Blood bilirubin increased.
• Blood bilirubin unconjugated increased.
• Blood cholinesterase abnormal.
• Blood cholinesterase decreased.
• Blood pressure decreased.
• Blood pressure diastolic decreased.
• Blood pressure systolic decreased.
• Blue toe syndrome.
• Brachiocephalic vein thrombosis.
• Brain stem embolism.
• Brain stem thrombosis.
• Bromosulphthalein test abnormal.
• Bronchial oedema.
• Bronchitis.
• Bronchitis mycoplasmal.
• Bronchitis viral.
• Bronchopulmonary aspergillosis allergic.
• Bronchospasm.
• Budd- Chiari syndrome.
• Bulbar palsy.
• Butterfly rash.
C
• C1q nephropathy.
• Caesarean section.
• Calcium embolism.
• Capillaritis.
• Caplan's syndrome.
• Cardiac amyloidosis.
• Cardiac arrest.
I had pv46663
— bob flaherty (@bobflaherty6) December 20, 2022
4 days later Hart attack pic.twitter.com/yeCQH2cMDK
• Cardiac failure.
• Cardiac failure acute.
• Cardiac sarcoidosis.
• Cardiac ventricular thrombosis.
• Cardiogenic shock.
• Cardiolipin antibody positive.
• Cardiopulmonary failure.
• Cardio-respiratory arrest.
• Cardio-respiratory distress.
• Cardiovascular insufficiency.
• Carotid arterial embolus.
• Carotid artery thrombosis.
• Cataplexy.
• Catheter site thrombosis.
• Catheter site vasculitis.
• Cavernous sinus thrombosis.
• CDKL5 deficiency disorder.
• CEC syndrome.
• Cement embolism.
• Central nervous system lupus.
• Central nervous system vasculitis.
• Cerebellar artery thrombosis.
• Cerebellar embolism.
• Cerebral amyloid angiopathy.
• Cerebral arteritis.
• Cerebral artery embolism.
• Cerebral artery thrombosis.
• Cerebral gas embolism.
• Cerebral microembolism.
• Cerebral septic infarct.
• Cerebral thrombosis.
• Cerebral venous sinus thrombosis.
Cerebral venous sinus thrombosis (CVST) is the presence of acute thrombosis - a blood clot in the dural venous sinuses which drain blood from the brain.
The main symptoms are: headaches, blurred vision, fainting or loss of consciousness, loss of control over movement in part of the body, seizures and coma.
• Cerebral venous thrombosis.
• Cerebrospinal thrombotic tamponade.
• Cerebrovascular accident.
A cerebrovascular accident (CVA), more commonly known as stroke is an acute compromise of the cerebral perfusion or vasculature. A stroke is a very serious condition where the blood supply to part of your brain is cut off. It needs to be treated in hospital as soon as possible.
Common symptoms of a stroke include your face dropping on one side, not being able to lift your arms and slurred speech. A stroke can be caused by either a blood clot in the brain or bleeding in the brain.
Below are USA VAERS stroke data, by age.
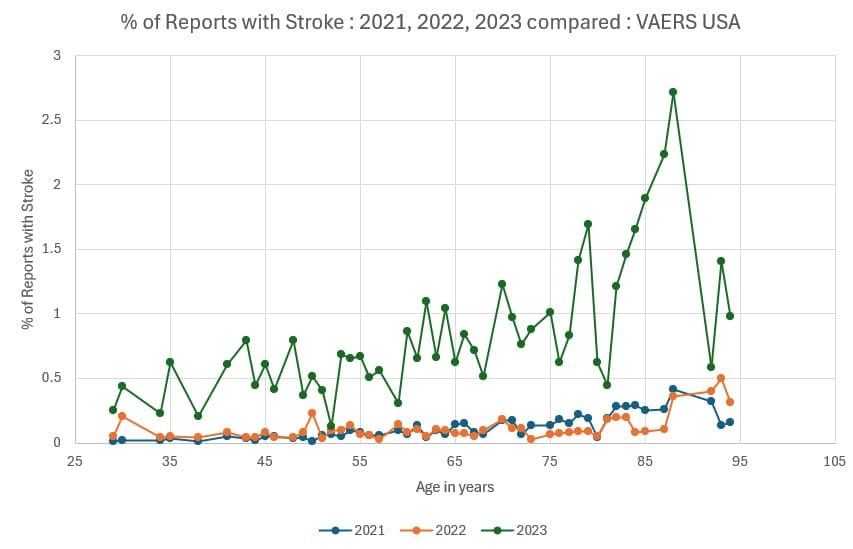
In 2021 and 2022 show about equal incidence, but 2023 excels.
• Change in seizure presentation.
• Chest discomfort.
• Child Pugh-Turcotte score abnormal.
• Child-Pugh-Turcotte score increased.
• Chillblains.
• Choking.
• Choking sensation.
• Cholangitis sclerosing.
• Chronic autoimmune glomerulonephritis.
• Chronic cutaneous lupus erythematosus.
• Chronic fatigue syndrome.
• Chronic gastritis.
• Chronic inflammatory demyelinating polyradiculoneuropathy.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is a neurological disorder characterised by progressive weakness and impaired sensory function in the legs and arms.
Simon Clark from Basildon, England replied back to Jules Serkin's tweet on Astrazeneca's batch on 19th December 2022. Clark has documented his experience with CIDP since taking the Covid-19 injection in March 2021.
I had this batch. 6 days later I was paralysed. I have chronic inflammatory demyelinating polyneuropathy and still bed bound pic.twitter.com/an3rtbm6ys
— Simon clark simonclark000.sc@googlemail (@Simonclark000Sc) December 20, 2022
CIDP is caused by an abnormal immune response and occurs when the immune system attacks the myelin covering of nerves. CIDP is thought to be an autoimmune disease. Health care providers also consider CIDP as the chronic form of Guillain-Barré Syndrome.
Symptoms include tingling, weakening and inability to feel pin prick in arms and legs. Loss of reflexes, balance and ability to walk.
• Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids.
• Chronic recurrent multifocal osteomyelitis.
• Chronic respiratory failure.
• Chronic spontaneous urticaria.
• Circulatory collapse.
• Circumoral oedema.
• Circumoral swelling.
• Clinically isolated syndrome.
• Clonic convulsion.
• Coeliac disease.
Coeliac disease is a condition where your immune system attacks your own tissues when you eat gluten. It stops you from taking in nutrients.
Symptoms of coeliac disease include diarrhoea, stomach aches and bloating. Coeliac disease is caused by the immune system attacking and damaging your gut when you eat food containing gluten.
• Cogan's syndrome.
• Cold agglutinins positive.
• Cold type haemolytic anaemia.
• Colitis.
• Colitis erosive.
• Colitis herpes.
• Colitis microscopic.
• Colitis ulcerative.
• Collagen disorder.
• Collagen-vascular disease.
• Complement factor abnormal.
• Complement factor C1 decreased.
• Complement factor C2 decreased.
• Complement factor C3 decreased.
• Complement factor C4 decreased.
• Complement factor decreased.
• Computerised tomogram liver abnormal.
• Concentric sclerosis.
• Congenital anomaly.
• Congenital bilateral perisylvian syndrome.
• Congenital herpes simplex infection.
• Congenital myasthenic syndrome.
• Congenital varicella infection.
• Congestive hepatopathy.
• Convulsion in childhood.
• Convulsions local.
• Convulsive threshold lowered.
• Coombs positive haemolytic anaemia.
• Coronary artery disease.
• Coronary artery embolism.
• Coronary artery thrombosis.
• Coronary bypass thrombosis.
• Coronavirus infection.
• Coronavirus test.
• Coronavirus test negative.
• Coronavirus test positive.
• Corpus callosotomy.
• Cough.
• Cough variant asthma.
• COVID-19.
• COVID-19 immunisation.
• COVID-19 pneumonia.
• COVID-19 prophylaxis.
• COVID-19 treatment.
• Cranial nerve disorder.
• Cranial nerve palsies multiple.
• Cranial nerve paralysis.
• CREST syndrome.
• Crohn's disease.
• Cryofibrinogenaemia.
• Cryoglobulinaemia
• CSF oligoclonal band present.
• CSWS syndrome.
• Cutaneous amyloidosis.
• Cutaneous lupus erythematosus.
• Cutaneous sarcoidosis.
• Cutaneous vasculitis.
• Cyanosis.
• Cyclic neutropenia.
• Cystitis interstitial.
• Cytokine release syndrome.
• Cytokine storm.
D
• De novo purine synthesis inhibitors associated acute inflammatory syndrome.
• Death neonatal.
• Deep vein thrombosis.
• Deep vein thrombosis postoperative.
• Deficiency of bile secretion.
• Deja vu.
• Demyelinating polyneuropathy.
• Demyelination.
• Dermatitis.
• Dermatitis bullous.
• Dermatitis herpetiformis.
• Dermatomyositis.
• Device embolisation.
• Device related thrombosis.
• Diabetes mellitus.
• Diabetic ketoacidosis.
• Diabetic mastopathy.
• Dialysis amyloidosis.
• Dialysis membrane reaction.
• Diastolic hypotension.
• Diffuse vasculitis.
• Digital pitting scar.
• Disseminated intravascular coagulation.
• Disseminated intravascular coagulation in newborn.
• Disseminated neonatal herpes simplex.
• Disseminated varicella.
• Disseminated varicella zoster vaccine virus infection.
• Disseminated varicella zoster virus infection.
• DNA antibody positive.
• Double cortex syndrome.
• Double stranded DNA antibody positive;Dreamy state.
• Dressler's syndrome.
• Drop attacks.
• Drug withdrawal convulsions.
• Dyspnoea.
• Early infantile epileptic encephalopathy with burst-suppression.
• Eclampsia.
• Eczema herpeticum.
• Embolia cutis medicamentosa.
• Embolic cerebellar infarction.
• Embolic cerebral infarction.
• Embolic pneumonia.
• Embolic stroke.
• Embolism.
• Embolism arterial.
• Embolism venous.
• Encephalitis.
• Encephalitis allergic.
• Encephalitis autoimmune.
• Encephalitis brain stem.
• Encephalitis haemorrhagic.
• Encephalitis periaxialis diffusa.
• Encephalitis post immunisation.
• Encephalomyelitis.
• Encephalopathy.
• Endocrine disorder.
• Endocrine ophthalmopathy.
• Endotracheal intubation.
• Enteritis.
• Enteritis leukopenic.
• Enterobacter pneumonia.
• Enterocolitis.
• Enteropathic spondylitis.
• Eosinopenia.
• Eosinophilic fasciitis.
• Eosinophilic granulomatosis with polyangiitis.
• Eosinophilic oesophagitis.
• Epidermolysis.
• Epilepsy.
• Epilepsy surgery.
• Epilepsy with myoclonic-atonic seizures.
• Epileptic aura.
• Epileptic psychosis.
• Erythema.
• Erythema induratum.
• Erythema multiforme.
• Erythema nodosum.
• Evans syndrome.
• Exanthema subitum.
• Expanded disability status scale score decreased.
• Expanded disability status scale score increased.
• Exposure to communicable disease.
• Exposure to SARS-CoV-2.
• Eye oedema.
• Eye pruritus.
• Eye swelling.
• Eyelid oedema.
F
• Face oedema.
• Facial paralysis.
• Facial paresis.
• Faciobrachial dystonic seizure.
• Fat embolism.
• Febrile convulsion.
• Febrile infection-related epilepsy syndrome.
• Febrile neutropenia.
• Felty's syndrome.
• Femoral artery embolism.
• Fibrillary glomerulonephritis.
• Fibromyalgia.
• Flushing.
• Foaming at mouth.
• Focal cortical resection.
• Focal dyscognitive seizures.
• Foetal distress syndrome.
• Foetal placental thrombosis.
• Foetor hepaticus.
• Foreign body embolism.
• Frontal lobe epilepsy.
• Fulminant type 1 diabetes mellitus.
G
• Galactose elimination capacity test abnormal.
• Galactose elimination capacity test decreased.
• Gamma-glutamyltransferase abnormal.
• Gamma-glutamyltransferase increased.
• Gastritis herpes.
• Gastrointestinal amyloidosis.
• Gelastic seizure.
• Generalised onset non-motor seizure.
• Generalised tonic-clonic seizure.
• Genital herpes.
• Genital herpes simplex.
• Genital herpes zoster.
• Giant cell arteritis.
• Glomerulonephritis.
• Glomerulonephritis membranoproliferative.
• Glomerulonephritis membranous.
• Glomerulonephritis rapidly progressive.
• Glossopharyngeal nerve paralysis.
• Glucose transporter type 1 deficiency syndrome.
• Glutamate dehydrogenase increased.
• Glycocholic acid increased.
• GM2 gangliosidosis.
• Goodpasture's syndrome.
• Graft thrombosis.
• Granulocytopenia.
• Granulocytopenia neonatal.
• Granulomatosis with polyangiitis.
• Granulomatous dermatitis.
• Grey matter heterotopia.
• Guanase increased
Giant Cell Arteritis (GCA) and Polymyalgia Rheumatica are two closely related inflammatory diseases that primarily affect individuals aged 50 years and older. GCA is a systemic large vessel vasculitis.
French reports of GCA, who developed their symptoms within one month of receiving COVID-19 vaccination (BNT162b2 mRNA (Pfizer- BioNTech), mRNA-1273 (Moderna),ChAdOx1 nCoV-19 Oxford-AstraZeneca), and Ad26.COV2.S (Johnson & Johnson/Janssen), between December 27th, 2020, and August 30th, 2022.
• Guillain Barre-syndrome.
Guillain-Barré syndrome (GBS) is also called acute inflammatory demyelinating polyradiculoneuropathy (AIDP). It is a neurological disorder in which the body's immune system attacks the peripheral nervous system, the part outside the brain and spinal cord.
My aunt was just diagnosed with a disease that literally eats away at her nerves and muscles and this is what it’s called. It’s because of the shots. pic.twitter.com/0Ok7iz8EfN
— IDIDNTDOIT (@IDIDNTDOIT2021) December 20, 2022
Symptons include muscle weakness, reflex loss, numbness or tingling in parts of body. It can lead to paralysis, which is usually temporary. Most people recover.
H
• Haemolytic anaemia.
• Haemophagocytic lymphohistiocytosis.
• Haemorrhage.
• Haemorrhagic ascites.
• Haemorrhagic disorder.
• Haemorrhagic pneumonia.
• Haemorrhagic varicella syndrome.
• Haemorrhagic vasculitis.
• Hantavirus pulmonary infection.
• Hashimoto's encephalopathy.
• Hashitoxicosis.
• Hemimegalencephaly.
• Henoch-Schonlein purpura.
Henoch-Schönlein purpura, now called immunoglobulin A (IgA) vasculitis, is an immune-mediated complex vasculitis. Henoch-Schönlein purpura affects capillary vessels and is characterized by the deposition of IgA on the walls of blood vessels. Clinical manifestations mainly involve cutaneous purpura, abdominal pain, arthritis, and nephropathy. The etiology of Henoch-Schönlein purpura is not completely understood, but it was observed following upper respiratory tract infections, medications and vaccinations.
The onset of Henoch-Schönlein purpura following coronavirus disease 2019 (COVID-19) infections and COVID-19 vaccines has been consistently reported from 2020 to date. This case report emphasises Henoch-Schönlein purpura was highly likely caused by the administration of COVID-19 vaccines since Henoch-Schönlein purpura had a temporal association with the messenger RNA (mRNA)-1273 (Moderna Inc.) administration, with no strong evidence for another cause.
A 22-year-old man visited the Dongkang Hospital in Ulsan with a rash on the lower limbs, bilateral ankle pain, and abdominal pain. He was admitted for spots on both feet and ankle pain, which started the day before visiting the hospital (Fig. 1).


Fig 1: Palpable purpura on lower limbs. Fig 2: (A) Day 1 of recurrence after improving symptoms and initiation of treatment with steroids. (B) Aggravated symptoms after discharge.
In this case, a young, healthy man without a medical history of upper respiratory infection and COVID-19 infection had purpura 18 days after being administered the mRNA-1273 vaccine. We can predict that the COVID-19 vaccine directly or indirectly affected the patient and precipitated Henoch-Schönlein purpura.
He had no remarkable medical history and was not on any medication. No signs of upper respiratory infection or COVID-19 infection were observed at admission. He had received the second dose of the mRNA COVID-19 vaccine mRNA-1273 (Moderna Inc.) 18 days before the visit. He did not have particular symptoms after receiving the first dose (mRNA-1273; Moderna Inc.).
According to a recent study by Ramdani published in March 2023, Henoch-Schönlein purpura reports have slightly increased in COVID-19 vaccines compared to all other drugs. However, no difference was observed between COVID-19 vaccines and other vaccines. A study demonstrated that COVID-19 vaccines did not differ from other vaccines as a factor that induces Henoch-Schönlein purpura.
• Henoch- Schonlein purpura nephritis.
• Hepaplastin abnormal.
• Hepaplastin decreased.
• Heparin-induced thrombocytopenia.
• Hepatic amyloidosis.
• Hepatic artery embolism.
• Hepatic artery flow decreased.
• Hepatic artery thrombosis.
• Hepatic enzyme abnormal.
• Hepatic enzyme decreased.
• Hepatic enzyme increased.
• Hepatic fibrosis marker abnormal.
• Hepatic fibrosis marker increased.
• Hepatic function abnormal.
• Hepatic hydrothorax.
• Hepatic hypertrophy.
• Hepatic hypoperfusion.
• Hepatic lymphocytic infiltration.
• Hepatic mass.
• Hepatic pain.
• Hepatic sequestration.
• Hepatic vascular resistance increased.
• Hepatic vascular thrombosis.
• Hepatic vein embolism.
• Hepatic vein thrombosis.
• Hepatic venous pressure gradient abnormal.
• Hepatic venous pressure gradient increased.
• Hepatitis.
• Hepatobiliary scan abnormal.
• Hepatomegaly.
• Hepatosplenomegaly.
• Hereditary angioedema with C1 esterase inhibitor deficiency.
• Herpes dermatitis.
• Herpes gestationis.
• Herpes oesophagitis.
• Herpes ophthalmic.
• Herpes pharyngitis.
• Herpes sepsis.
• Herpes simplex.
• Herpes simplex cervicitis.
• Herpes simplex colitis.
• Herpes simplex encephalitis.
• Herpes simplex gastritis.
• Herpes simplex hepatitis.
• Herpes simplex meningitis.
• Herpes simplex meningoencephalitis.
• Herpes simplex meningomyelitis.
• Herpes simplex necrotising retinopathy.
• Herpes simplex oesophagitis.
• Herpes simplex otitis externa.
• Herpes simplex pharyngitis.
• Herpes simplex pneumonia.
• Herpes simplex reactivation.
• Herpes simplex sepsis.
• Herpes simplex viraemia.
• Herpes simplex virus conjunctivitis neonatal.
• Herpes simplex visceral.
• Herpes virus infection.
• Herpes zoster.
• Herpes zoster cutaneous disseminated.
• Herpes zoster infection neurological.
• Herpes zoster meningitis.
• Herpes zoster meningoencephalitis.
• Herpes zoster meningomyelitis.
• Herpes zoster meningoradiculitis.
• Herpes zoster necrotising retinopathy.
• Herpes zoster oticus (Ramsay Hunt Syndrome.)
Symptoms of Ramsey Hunt syndrome can include pain, vertigo, hearing loss, sensitivity to sound, tinnitus (a chronic ringing in the ears), loss of taste, a change in taste sensation, dry eye, tearing, hyperacusis, nasal obstruction, and dysarthria.
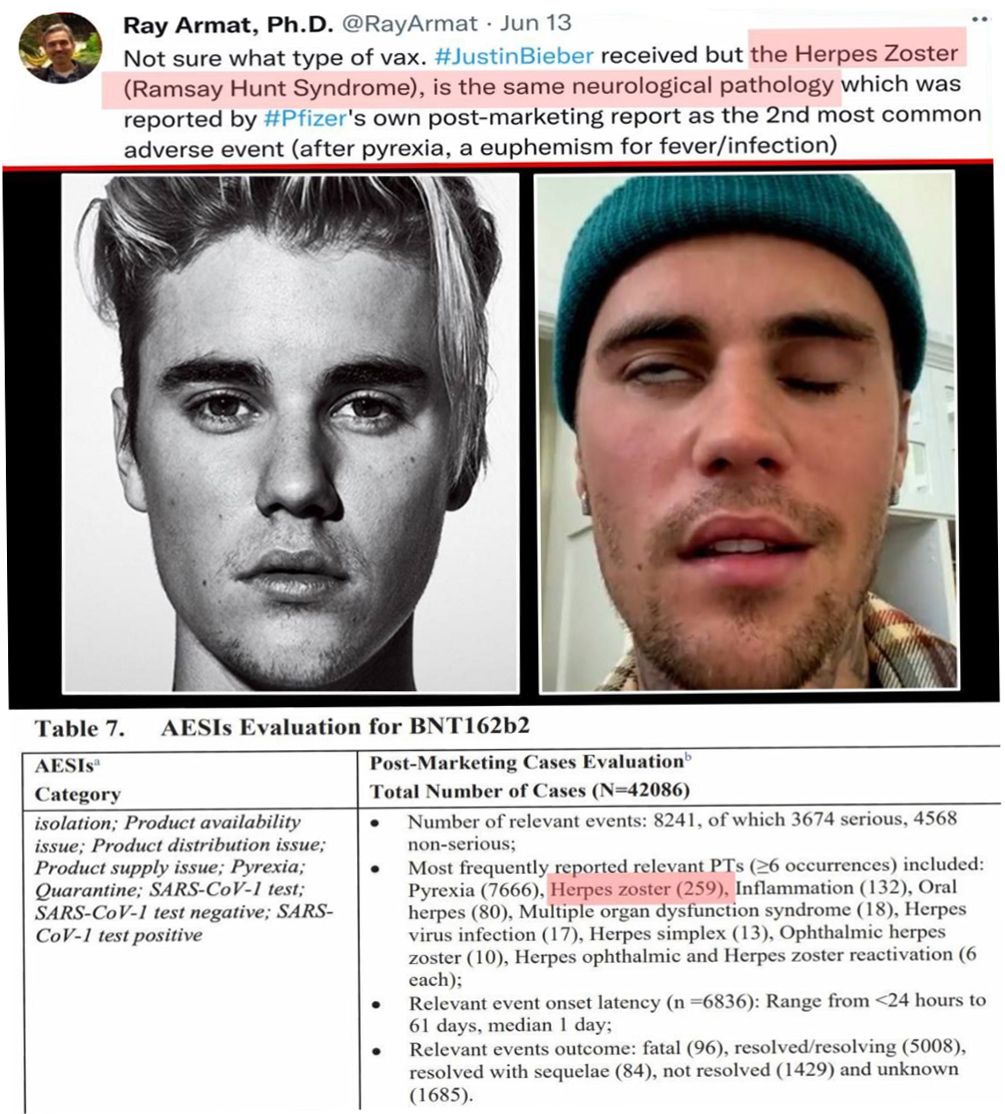
Ramsay Hunt syndrome is the second most common cause of facial palsy. The disease progresses rapidly in 2-3 days. Patients complain of difficulty in closing eye and facial weakness.
• Herpes zoster pharyngitis.
• Herpes zoster reactivation.
• Herpetic radiculopathy.
• Histone antibody positive.
• Hoigne's syndrome.
• Human herpesvirus 6 encephalitis.
• Human herpesvirus 6 infection.
• Human herpesvirus 6 infection reactivation.
• Human herpesvirus 7 infection.
• Human herpesvirus 8 infection.
• Hyperammonaemia.
• Hyperbilirubinaemia.
• Hypercholia.
• Hypergammaglobulinaemia benign monoclonal.
• Hyperglycaemic seizure.
• Hypersensitivity.
• Hypersensitivityvasculitis.
• Hyperthyroidism.
• Hypertransaminasaemia.
• Hyperventilation.
• Hypoalbuminaemia.
• Hypocalcaemic seizure.
• Hypogammaglobulinaemia.
• Hypoglossal nerve paralysis.
• Hypoglossal nerve paresis.
• Hypoglycaemic seizure.
• Hyponatraemic seizure.
• Hypotension.
• Hypotensive crisis.
• Hypothenar hammer syndrome.
• Hypothyroidism.
• Hypoxia.
I
• Idiopathic CD4 lymphocytopenia.
• Idiopathic generalised epilepsy.
• Idiopathic interstitial pneumonia.
• Idiopathic neutropenia.
• Idiopathic pulmonary fibrosis.
• IgA nephropathy.
• IgM nephropathy.
• IIIrd nerve paralysis.
• IIIrd nerve paresis.
• Iliac artery embolism.
• Immune thrombocytopenia.
• Immune-mediated adverse reaction.
• Immune-mediated cholangitis.
• Immune-mediated cholestasis.
• Immune-mediated cytopenia.
• Immune-mediated encephalitis.
• Immune-mediated encephalopathy.
• Immune-mediated endocrinopathy.
• Immune-mediated enterocolitis.
• Immune-mediated gastritis.
• Immune-mediated hepatic disorder.
• Immune-mediated hepatitis.
• Immune-mediated hyperthyroidism.
• Immune-mediated hypothyroidism.
• Immune-mediated myocarditis.
• Immune-mediated myositis.
• Immune-mediated nephritis.
• Immune-mediated neuropathy.
• Immune-mediated pancreatitis.
• Immune-mediated pneumonitis.
• Immune-mediated renal disorder.
• Immune-mediated thyroiditis.
• Immune-mediated uveitis.
• Immunoglobulin G4 related disease;.
• Immunoglobulins abnormal.
• Implant site thrombosis.
• Inclusion body myositis.
• Infantile genetic agranulocytosis.
• Infantile spasms.
• Infected vasculitis.
• Infective thrombosis.
• Inflammation.
• Inflammatory bowel disease.
• Infusion site thrombosis.
• Infusion site vasculitis.
• Injection site thrombosis.
• Injection site urticaria.
• Injection site vasculitis.
• Instillation site thrombosis.
• Insulin autoimmune syndrome.
• Interstitial granulomatous dermatitis.
• Interstitial lung disease.
• Intracardiac mass.
• Intracardiac thrombus.
• Intracranial pressure increased.
• Intrapericardial thrombosis.
• Intrinsic factor antibody abnormal.
• Intrinsic factor antibody positive.
• IPEX syndrome.
• Irregular breathing.
• IRVAN syndrome.
• IVth nerve paralysis.
• IVth nerve paresis.
J
• JC polyomavirus test positive.
• JC virus CSF test positive.
• Jeavons syndrome.
• Jugular vein embolism.
• Jugular vein thrombosis.
• Juvenile idiopathic arthritis.
• Juvenile myoclonic epilepsy.
• Juvenile polymyositis.
• Juvenile psoriatic arthritis.
• Juvenile spondyloarthritis.
K
• Kaposi sarcoma inflammatory cytokine syndrome.
• Kawasaki's disease.
• Kayser-Fleischer ring.
• Keratoderma blenorrhagica.
• Ketosis-prone diabetes mellitus.
• Kounis syndrome.
L
• Lafora's myoclonic epilepsy.
• Lambl's excrescences.
• Laryngeal dyspnoea.
• Laryngeal oedema.
• Laryngeal rheumatoid arthritis.
• Laryngospasm.
• Laryngotracheal oedema.
• Latent autoimmune diabetes in adults.
• LE cells present.
• Lemierre syndrome.
• Lennox-Gastaut syndrome.
• Leucine aminopeptidase increased.
• Leukoencephalomyelitis.
• Leukoencephalopathy.
• Leukopenia.
• Leukopenia neonatal.
• Lewis-Sumner syndrome.
• Lhermitte's sign.
• Lichen planopilaris.
• Lichen planus.
• Lichen sclerosus.
• Limbic encephalitis.
• Linear IgA disease.
• Lip oedema.
• Lip swelling.
• Liver function test abnormal.
• Liver function test decreased.
• Liver function test increased.
• Liver induration.
• Liver injury.
• Liver iron concentration abnormal.
• Liver iron concentration increased.
• Liver opacity.
• Liver palpable.
• Liver sarcoidosis.
• Liver scan abnormal.
• Liver tenderness.
• Low birth weight baby.
• Lower respiratory tract herpes infection.
• Lower respiratory tract infection.
• Lower respiratory tract infection viral.
• Lung abscess.
• Lupoid hepatic cirrhosis.
• Lupus cystitis.
• Lupus encephalitis.
• Lupus endocarditis.
• Lupus enteritis.
• Lupus hepatitis.
• Lupus myocarditis.
• Lupus myositis.
• Lupus nephritis.
• Lupus pancreatitis.
• Lupus pleurisy.
• Lupus pneumonitis.
• Lupus vasculitis.
• Lupus-like syndrome.
• Lymphocytic hypophysitis.
• Lymphocytopenia neonatal.
• Lymphopenia.
M
• MAGIC syndrome.
• Magnetic resonance imaging liver abnormal.
• Magnetic resonance proton density fat fraction measurement.
• Mahler sign.
• Manufacturing laboratory analytical testing issue.
• Manufacturing materials issue.
• Manufacturing production issue.
• Marburg's variant multiple sclerosis.
• Marchiafava-Bignami diseas.
• Marine Lenhart syndrome.
• Mastocytic enterocolitis.
• Maternal exposure during pregnancy.
• Medical device site thrombosis.
• Medical device site vasculitis.
• MELAS syndrome.
• Meningitis.
• Meningitis aseptic.
• Meningitis herpes.
• Meningoencephalitis herpes simplex neonatal.
• Meningoencephalitis herpetic.
• Meningomyelitis herpes.
• MERS-CoV test.
• MERS-CoV test negative.
• MERS-CoV test positive.
• Mesangioproliferative glomerulonephritis.
• Mesenteric artery embolism.
• Mesenteric artery thrombosis.
• Mesenteric vein thrombosis.
• Metapneumovirus infection.
• Metastatic cutaneous Crohn's disease.
• Metastatic pulmonary embolism.
• Microangiopathy.
• Microembolism.
• Microscopic polyangiitis.
• Middle East respiratory syndrome.
• Migraine-triggered seizure.
• Miliary pneumonia.
• Miller Fisher syndrome.
• Mitochondrial aspartate aminotransferase increased.
• Mixed connective tissue disease.
• Model for end stage liver disease score abnormal.
• Model for end stage liver disease score increased.
• Molar ratio of total branched-chain amino acid to tyrosine.
• Molybdenum cofactor deficiency.
• Monocytopenia.
• Mononeuritis.
• Mononeuropathy multiplex.
• Morphoea.
• Morvan syndrome.
• Mouth swelling.
• Moyamoya disease.
• Multifocal motor neuropathy.
• Multiple organ dysfunction syndrome.
• Multiple sclerosis.
• Multiple sclerosis relapse.
• Multiple sclerosis relapse prophylaxis.
• Multiple subpial transection.
• Multisystem inflammatory syndrome in children.
• Muscular sarcoidosis.
• Myasthenia gravis.
• Myasthenia gravis crisis.
• Myasthenia gravis neonatal.
• Myasthenic syndrome.
• Myelitis.
• Myelitis transverse.
• Myocardial infarction.
• Myocarditis.
Myocarditis after COVID-19 vaccination. Download clinical case report of 37 year old woman below.
The subject was hospitalized following the manifestation of fatigue, dyspnea, and peripheral edema. It was observed that her symptoms began 4 days after receiving her second mRNA COVID-19 vaccination (BNT162b2).

The below chart for myocarditis is differs from charts for other cardio-vascular disorders. Here, the highest incidence is in younger age groups, suggesting an autoimmune attack.
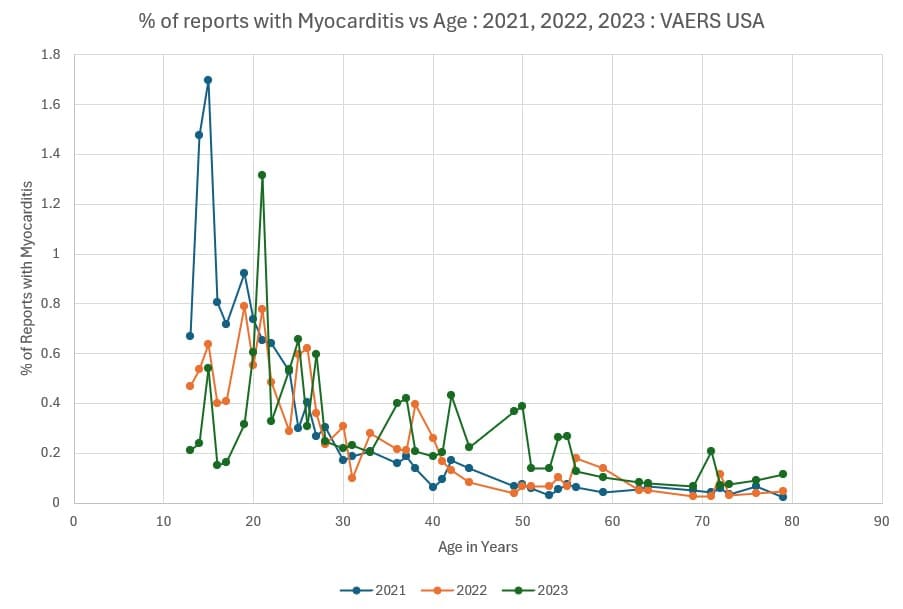
If the heart is harder to regenerate, then a stronger autoimmune attack in younger age groups may result in a higher level of heart damage in the young.
• Myocarditis post infection.
• Myoclonic epilepsy.
• Myoclonic epilepsy and ragged-red fibres.
• Myokymia.
• Myositis.
N
• Narcolepsy.
• Nasal herpes.
• Nasal obstruction.
• Necrotising herpetic retinopathy.
• Neonatal Crohn's disease.
• Neonatal epileptic seizure.
• Neonatal lupus erythematosus.
• Neonatal mucocutaneous herpes simplex.
• Neonatal pneumonia.
• Neonatal seizure.
• Nephritis.
• Nephrogenic systemic fibrosis.
• Neuralgic amyotrophy.
• Neuritis.
• Neuritis cranial.
• Neuromyelitis optica pseudo relapse.
• Neuromyelitis optica spectrum disorder.
• Neuromyotonia;Neuronal neuropathy.
• Neuropathy peripheral.
• Neuropathy ataxia retinitis pigmentosa syndrome.
• Neuropsychiatric lupus.
• Neurosarcoidosis.
• Neutropenia.
• Neutropenia neonatal.
• Neutropenic colitis.
• Neutropenic infection.
• Neutropenic sepsis.
• Nodular rash.
• Nodular vasculitis.
• Noninfectious myelitis.
• Noninfective encephalitis.
• Noninfective encephalomyelitis.
• Noninfective oophoritis.
O
• Obstetrical pulmonary embolism.
• Occupational exposure to communicable disease.
• Occupational exposure to SARS-CoV-2;Ocular hyperaemia.
• Ocular myasthenia.
• Ocular pemphigoid.
• Ocular sarcoidosis.
• Ocular vasculitis.
• Oculofacial paralysis.
• Oedema.
• Oedema blister.
• Oedema due to hepatic disease.
• Oedema mouth.
• Oesophageal achalasia.
• Ophthalmic artery thrombosis.
• Ophthalmic herpes simplex.
• Ophthalmic herpes zoster.
• Ophthalmic vein thrombosis.
• Optic neuritis.
• Optic neuropathy.
• Optic perineuritis.
• Oral herpes.
• Oral lichen planus.
• Oropharyngeal oedema.
• Oropharyngeal spasm.
• Oropharyngeal swelling.
• Osmotic demyelination syndrome.
• Ovarian vein thrombosis.
• Overlap syndrome.
P
• Paediatric autoimmune neuropsychiatric disorders associated with streptococcal infection.
• Paget-Schroetter syndrome.
• Palindromic rheumatism.
• Palisaded neutrophilic granulomatous dermatitis.
• Palmoplantar keratoderma.
• Palpable purpura.
• Pancreatitis.
• Panencephalitis.
• Papillophlebitis.
• Paracancerous pneumonia.
• Paradoxical embolism.
• Parainfluenzae viral laryngotracheobronchitis.
• Paraneoplastic dermatomyositis.
• Paraneoplastic pemphigus.
• Paraneoplastic thrombosis.
• Paresis cranial nerve.
• Parietal cell antibody positive.
• Paroxysmal nocturnal haemoglobinuria.
• Partial seizures.
• Partial seizures with secondary generalisation.
• Patient isolation.
• Pelvic venous thrombosis.
• Pemphigoid;Pemphigus.
• Penile vein thrombosis.
• Pericarditis.
• Pericarditis lupus.
• Perihepatic discomfort.
• Periorbital oedema.
• Periorbital swelling.
• Peripheral artery thrombosis.
• Peripheral embolism.
• Peripheral ischaemia.
• Peripheral vein thrombus extension.
• Periportal oedema.
• Peritoneal fluid protein abnormal.
• Peritoneal fluid protein decreased.
• Peritoneal fluid protein increased.
• Peritonitis lupus.
• Pernicious anaemia.
• Petit mal epilepsy.
• Pharyngeal oedema.
• Pharyngeal swelling.
• Pityriasis lichenoides et varioliformis acuta.
• Placenta praevia.
• Pleuroparenchymal fibroelastosis.
• Pneumobilia.
• Pneumonia.
• Pneumonia adenoviral.
• Pneumonia cytomegaloviral.
• Pneumonia herpes viral.
• Pneumonia influenzal.
• Pneumonia measles.
• Pneumonia mycoplasmal.
• Pneumonia necrotising.
• Pneumonia parainfluenzae viral.
• Pneumonia respiratory syncytial viral.
• Pneumonia viral.
• POEMS syndrome.
• Polyarteritis nodosa.
• Polyarthritis.
• Polychondritis.
• Polyglandular autoimmune syndrome type I.
• Polyglandular autoimmune syndrome type II.
• Polyglandular autoimmune syndrome type III.
• Polyglandular disorder.
• Polymicrogyria.
• Polymyalgia rheumatica.
• Polymyositis.
• Polyneuropathy.
• Polyneuropathy idiopathic progressive.
• Portal pyaemia.
• Portal vein embolism.
• Portal vein flow decreased.
• Portal vein pressure increased.
• Portal vein thrombosis.
• Portosplenomesenteric venous thrombosis.
• Post procedural hypotension.
• Post procedural pneumonia.
• Post procedural pulmonary embolism.
• Post stroke epilepsy.
• Post stroke seizure.
• Post thrombotic retinopathy.
• Post thrombotic syndrome.
• Post viral fatigue syndrome.
• Postictal headache.
• Postictal paralysis.
• Postictal psychosis.
• Postictal state.
• Postoperative respiratory distress.
• Postoperative respiratory failure.
• Postoperative thrombosis.
• Postpartum thrombosis.
• Postpartum venous thrombosis.
• Postpericardiotomy syndrome.
• Post-traumatic epilepsy.
• Postural orthostatic tachycardia syndrome.
• Precerebral artery thrombosis.
• Pre-eclampsia.
• Preictal state.
• Premature labour.
• Premature menopause.
• Primary amyloidosis.
• Primary biliary cholangitis.
• Primary progressive multiple sclerosis.
• Procedural shock.
• Proctitis herpes.
• Proctitis ulcerative.
• Product availability issue;Product distribution issue.
• Product supply issue.
• Progressive facial hemiatrophy.
• Progressive multifocal leukoencephalopathy.
• Progressive multiple sclerosis.
• Progressive relapsing multiple sclerosis.
• Prosthetic cardiac valve thrombosis.
• Pruritus.
• Pruritus allergic.
• Pseudovasculitis.
• Psoriasis.
• Psoriatic arthropathy.
• Pulmonary amyloidosis.
• Pulmonary artery thrombosis.
• Pulmonary embolism.
• Pulmonary fibrosis.
• Pulmonary haemorrhage.
• Pulmonary microemboli.
• Pulmonary oil microembolism.
• Pulmonary renal syndrome.
• Pulmonary sarcoidosis.
• Pulmonary sepsis.
• Pulmonary thrombosis.
• Pulmonary tumour thrombotic microangiopathy.
Pulmonary Tumor Thrombotic Microangiopathy (PTTM) is a condition that can lead to acute severe pulmonary hypertension and circulatory failure. Caused by tumor cell microvascular obstruction and is usually difficult to diagnose; often diagnosed after death.
This case report is from a patient who died 15 days after onset of the disease.
A 61-year-old female with no relevant medical history presented to a hospital with sudden dyspnea. She received a Pfizer-BioNTech BNT162b2 mRNA injection two days before onset.
Contrast-enhanced CT showed no obvious contrast deficit in the pulmonary artery. Her hemodynamics deteriorated during the examination, leading to cardiac arrest. The patient was treated with venoarterial extracorporeal membrane oxygenation (VA-ECMO) via the femoral artery and vein, and her heartbeat resumed. She was transferred to our hospital for further treatment.
Blood tests revealed an elevated inflammatory response and liver and renal dysfunction.
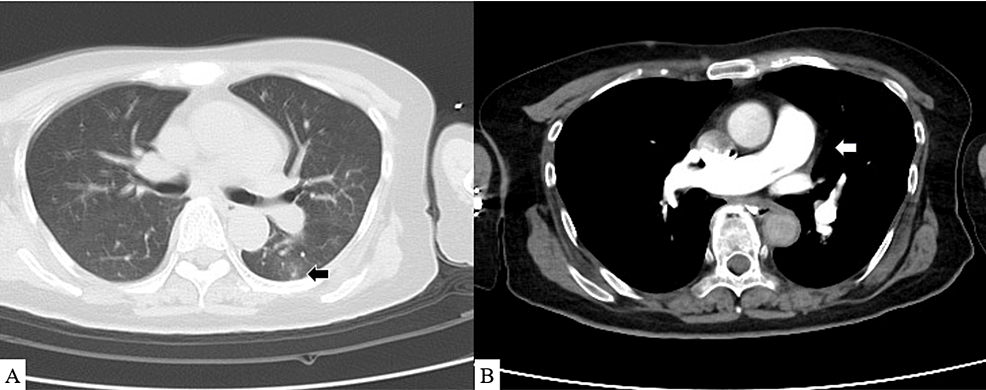
COVID-19 vaccine-related myocarditis was suspected given sudden post-vaccine severe cardiac decompensation, and steroid pulse therapy and high-dose gamma globulin treatments were initiated.
Nitric oxide therapy for pulmonary hypertension was initiated, and an Impella heart pump fitted.
A myocardial biopsy was performed as well. On the seventh day, the flow through the Impella heart pump dropped and could not be maintained despite the reduction in the ECMO flow. The heart pump was removed. Transesophageal electrocardiography showed further RV enlargement and LV collapse.
This seemed insufficient for blood flow from the right to the left heart system. A myocardial biopsy revealed no significant inflammatory cellular infiltrates or evidence of amyloidosis or sarcoidosis. Chest radiography revealed severe pulmonary congestion. Follow-up CT showed the worsening of the lung field consolidation, and contrast defects of the pulmonary arteries remained absent.
• Pulmonary vasculitis.
• Pulmonary veno-occlusive disease.
• Pulmonary venous thrombosis.
• Pyoderma gangrenosum.
• Pyostomatitis vegetans.
• Pyrexia.
Q
• Quarantine.
R
• Radiation leukopenia.
• Radiculitis brachial.
• Radiologically isolated syndrome.
• Rash.
• Rash erythematous.
• Rash pruritic.
• Rasmussen encephalitis.
• Raynaud's phenomenon.
• Reactive capillary endothelial proliferation.
• Relapsing multiple sclerosis.
• Relapsing-remitting multiple sclerosis.
• Renal amyloidosis.
• Renal arteritis.
• Renal artery thrombosis.
• Renal embolism.
• Renal failure.
• Renal vascular thrombosis.
• Renal vasculitis.
• Renal vein embolism.
• Renal vein thrombosis.
• Respiratory arrest.
• Respiratory disorder.
• Respiratory distress.
• Respiratory failure.
• Respiratory paralysis.
• Respiratory syncytial virus bronchiolitis.
• Respiratory syncytial virus bronchitis.
• Retinal artery embolism.
• Retinal artery occlusion.
• Retinal artery thrombosis.
• Retinal vascular thrombosis.
• Retinal vasculitis.
• Retinal vein occlusion.
• Retinal vein thrombosis.
• Retinol binding protein decreased.
• Retinopathy.
• Retrograde portal vein flow.
• Retroperitoneal fibrosis.
• Reversible airways obstruction.
• Reynold's syndrome.
• Rheumatic brain disease.
• Rheumatic disorder.
• Rheumatoid arthritis.
• Rheumatoid factor increased.
• Rheumatoid factor positive.
• Rheumatoid factor quantitative increased.
• Rheumatoid lung.
• Rheumatoid neutrophilic dermatosis.
• Rheumatoid nodule.
• Rheumatoid nodule removal.
• Rheumatoid scleritis.
• Rheumatoid vasculitis.
S
• Saccadic eye movement.
• SAPHO syndrome.
• Sarcoidosis.
• SARS-CoV-1 test.
• SARS-CoV-1 test negative.
• SARS-CoV-1 test positive.
• SARS-CoV-2 antibody test.
• SARS-CoV-2 antibody test negative.
• SARS-CoV-2 antibody test positive.
• SARS-CoV-2 carrier.
• SARS-CoV-2 sepsis.
• SARS-CoV-2 test.
• SARS- CoV-2 test false negative.
• SARS-CoV-2 test false positive.
• SARS-CoV-2 test negative.
• SARS- CoV-2 test positive.
• SARS-CoV-2 viraemia.
• Satoyoshi syndrome.
• Schizencephaly.
• Scleritis.
• Sclerodactylia.
• Scleroderma.
• Scleroderma associated digital ulcer.
• Scleroderma renal crisis.
• Scleroderma-like reaction.
• Secondary amyloidosis.
• Secondary cerebellar degeneration.
• Secondary progressive multiple sclerosis.
• Segmented hyalinising vasculitis.
• Seizure.
• Seizure anoxic.
• Seizure cluster.
• Seizure like phenomena.
• Seizure prophylaxis.
• Sensation of foreign body.
• Septic embolus.
• Septic pulmonary embolism.
• Severe acute respiratory syndrome.
• Severe myoclonic epilepsy of infancy.
• Shock.
• Shock symptom.
• Shrinking lung syndrome.
• Shunt thrombosis.
• Silent thyroiditis.
• Simple partial seizures.
• Sjogren's syndrome.
• Skin swelling.
• SLE arthritis.
• Smooth muscle antibody positive.
• Sneezing.
• Spinal artery embolism.
• Spinal artery thrombosis.
• Splenic artery thrombosis.
• Splenic embolism.
• Splenic thrombosis.
• Splenic vein thrombosis.
• Spondylitis.
• Spondyloarthropathy.
• Spontaneous heparin-induced thrombocytopenia syndrome.
• Status epilepticus.
• Stevens-Johnson syndrome.
Stevens-Johnson syndrome (SJS) is an acute hypersensitivity reaction that causes extensive necrosis of the mucous membrane and skin. SJS results from a cytotoxic immune reaction in keratinocytes, which leads to widespread keratinocyte apoptosis.
A middle-aged female patient came to the College of Dentistry, Taibah University, Saudi Arabia, 5 days after the second dose of the COVID-19 Pfizer vaccine, complaining of large, red-colored bullae at the left retromolar area (Figure 1) that ruptured and refilled.
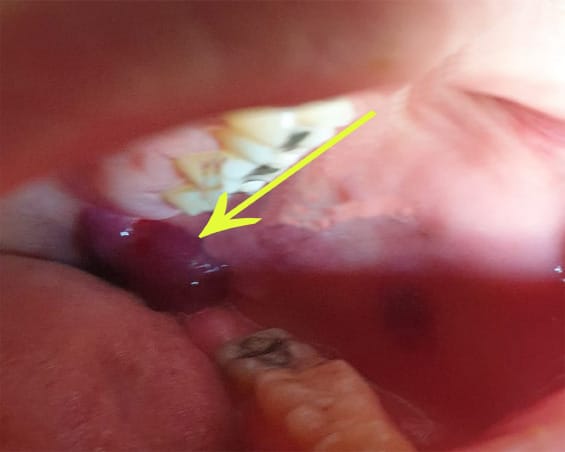


Fig. 1 Large, deep-red bullae at retromolar area. Fig. 2 Large oral ulcerations at labial mucosa with yellow crust at lower lip. Fig. 3 Multiple large oral ulcerations at buccal mucosa.
The patient reported that she had taken the second dose of the BNT162b1 SARS-CoV-2 vaccine 5 days previously. The patient reported that she had a mild fever and general weakness. A D-dimer test was done to detect the possibility of blood clots. Laboratory examination of the D-dimer test showed a slight elevation with 0.63 mg/L.
• Stiff leg syndrome.
• Stiff Person Syndrome.
Stiff Person Syndrome (SPS) is a progressive neurological disease. Symptoms include stiff muscles in the torso, arms, legs and greater sensitivity to noise, touch and emotional distress.
Celine Dion
People with SPS may develop abnormal, often hunched over postures, unable to walk or move. Many fall frequently, not having the normal reflexes to catch themselves.
• Stillbirth.
• Still's disease.
• Stoma site thrombosis.
• Stoma site vasculitis.
• Stress cardiomyopathy.
• Stridor.
• Subacute cutaneous lupus erythematosus.
• Subacute endocarditis.
• Subacute inflammatory demyelinating polyneuropathy.
• Subclavian artery embolism.
• Subclavian artery thrombosis.
• Subclavian vein thrombosis.
• Sudden unexplained death in epilepsy.
• Superior sagittal sinus thrombosis.
• Susac's syndrome.
• Suspected COVID- 19.
• Swelling.
• Swelling face.
• Swelling of eyelid.
• Swollen tongue.
• Sympathetic ophthalmia.
• Systemic lupus erythematosus.
• Systemic lupus erythematosus disease activity index abnormal.
• Systemic lupus erythematosus disease activity index decreased.
• Systemic lupus erythematosus disease activity index increased.
• Systemic lupus erythematosus rash;Systemic scleroderma.
• Systemic sclerosis pulmonary.
T
• Tachycardia.
• Tachypnoea.
• Takayasu's arteritis.
• Temporal lobe epilepsy.
• Terminal ileitis.
• Testicular autoimmunity.
• Throat tightness.
• Thromboangiitis obliterans.
• Thrombocytopenia.
• Thrombocytopenic purpura.
• Thrombophlebitis.
• Thrombophlebitis migrans.
• Thrombophlebitis neonatal.
• Thrombophlebitis septic.
• Thrombophlebitis superficial.
• Thromboplastin antibody positive.
• Thrombosis.
• Thrombosis corpora cavernosa.
• Thrombosis in device.
• Thrombosis mesenteric vessel.
• Thrombotic cerebral infarction.
• Thrombotic microangiopathy.
• Thrombotic stroke.
• Thrombotic thrombocytopenic purpura.
• Thyroid disorder.
• Thyroid stimulating immunoglobulin increased.
• Thyroiditis.
• Tongue amyloidosis.
• Tongue biting.
• Tongue oedema.
• Tonic clonic movements.
• Tonic convulsion.
• Tonic posturing.
• Topectomy.
• Total bile acids increased.
• Toxic epidermal necrolysis.
• Toxic leukoencephalopathy.
• Toxic oil syndrome.
• Tracheal obstruction.
• Tracheal oedema.
• Tracheobronchitis.
• Tracheobronchitis mycoplasmal.
• Tracheobronchitis viral.
• Transaminases abnormal.
• Transaminases increased.
• Transfusion-related alloimmune neutropenia.
• Transient epileptic amnesia.
• Transverse sinus thrombosis.
• Trigeminal nerve paresis.
• Trigeminal neuralgia.
• Trigeminal palsy.
• Truncus coeliacus thrombosis.
• Tuberous sclerosis complex.
• Tubulointerstitial nephritis and uveitis syndrome.
• Tumefactive multiple sclerosis.
• Tumour embolism.
• Tumour thrombosis.
• Type 1 diabetes mellitus.
• Type I hypersensitivity.
• Type III immune complex mediated reaction.
U
• Uhthoff's phenomenon.
• Ulcerative keratitis.
• Ultrasound liver abnormal.
• Umbilical cord thrombosis.
• Uncinate fits.
• Undifferentiated connective tissue disease.
• Upper airway obstruction.
• Urine bilirubin increased.
• Urobilinogen urine decreased.
• Urobilinogen urine increased.
• Urticaria;Urticaria papular.
• Urticarial vasculitis.
• Uterine rupture.
• Uveitis.
V
• Vaccination site thrombosis.
• Vaccination site vasculitis.
• Vagus nerve paralysis.
• Varicella.
• Varicella keratitis.
• Varicella post vaccine.
• Varicella zoster gastritis.
• Varicella zoster oesophagitis.
• Varicella zoster pneumonia.
• Varicella zoster sepsis.
• Varicella zoster virus infection.
• Vasa praevia.
• Vascular graft thrombosis.
• Vascular pseudoaneurysm thrombosis.
• Vascular purpura.
• Vascular stent thrombosis.
• Vasculitic rash.
• Vasculitic ulcer.
• Vasculitis.
• Vasculitis gastrointestinal.
• Vasculitis necrotising.
• Vena cava embolism.
• Vena cava thrombosis.
• Venous intravasation.
• Venous recanalisation.
• Venous thrombosis.
• Venous thrombosis in pregnancy.
• Venous thrombosis limb.
• Venous thrombosis neonatal.
• Vertebral artery thrombosis.
• Vessel puncture site thrombosis.
• Visceral venous thrombosis.
• VIth nerve paralysis.
• VIth nerve paresis;Vitiligo.
• Vocal cord paralysis.
• Vocal cord paresis.
• Vogt-Koyanagi-Harada disease.
Vogt–Koyanagi–Harada (VKH) disease is a chronic systemic inflammatory disorder characterized by bilateral panuveitis.1 It is associated with serous retinal detachments, disk edema, and vitritis with eventual development of sunset glow fundus.
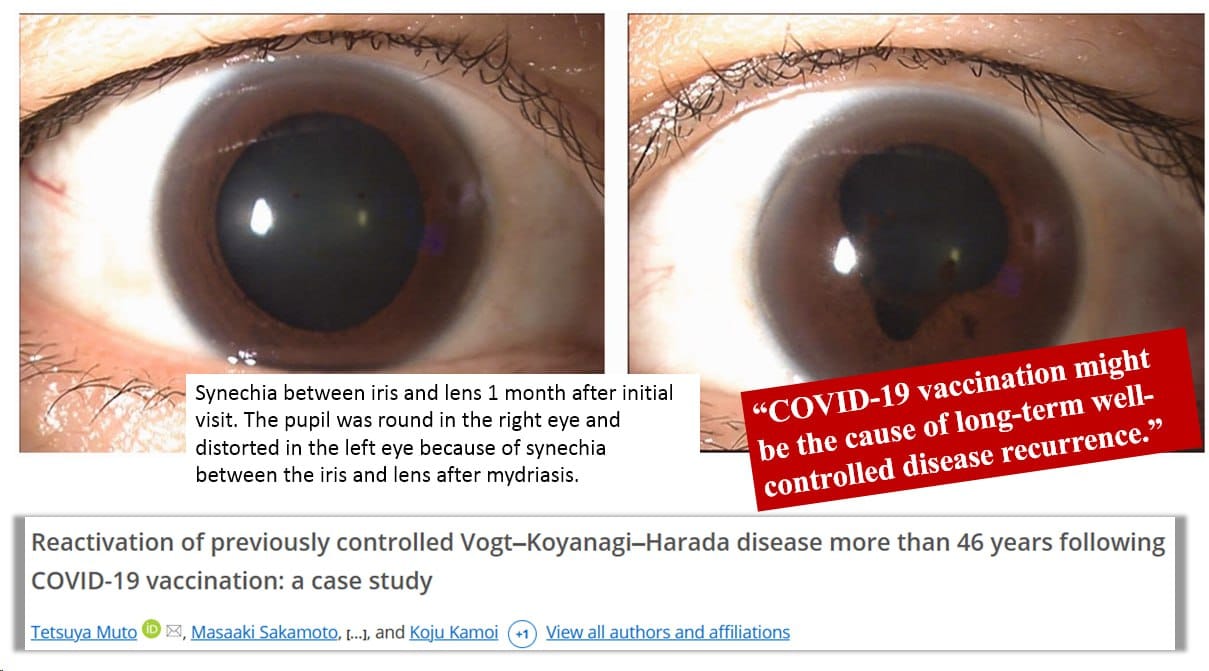
Papasavvas and Herbort reported a case involving the post-COVID-19 vaccination recurrence of VKH disease that had been controlled for >6 years; the recurrence developed 6 weeks after administration of the second dose of the Pfizer COVID-19 vaccine.
Accorinti reported a case of recurrence of well-controlled VKH disease 11 days after the first dose of the Pfizer COVID-19 vaccine. Bolletta reported that the mean time between vaccination and onset of ocular complications was 9.4 days.
Rujkorakarn and Patamatamkul reported the recurrence of VKH disease 1 week after the third dose of an mRNA-based vaccine (mRNA-1273; Moderna). Our patient developed blurred vision 2 months after the third dose of the Pfizer COVID-19 vaccination, whereas Yasaka defined ocular complications as the development of ocular inflammatory events within 14 days after COVID-19 vaccination.
W
• Warm type haemolytic anaemia.
• Wheezing.
• White nipple sign.
X
• XIth nerve paralysis.
• X-ray hepatobiliary abnormal.
Y
• Young's syndrome.
Z
• Zika virus associated Guillain Barre syndrome.